There is no clear conclusion on which dialysis method should be used in end-stage diabetic nephropathy. Peritoneal dialysis therapy has less impact on the cardiovascular system and better protection of residual renal function than hemodialysis, and may be more suitable for some patients with diabetic nephropathy.
Timing of peritoneal dialysis initiation in patients with diabetic nephropathy
In view of the specificity of end-stage diabetic nephropathy, dialysis treatment should be earlier than non-diabetic patients. In the absence of intestinal infection, diverticulum, severe peritoneal adhesions, etc., the pre-dialysis preparation can be started when the glomerular filtration rate (GFR) drops to 20-30 ml/min, and dialysis can be started when GFR is less than 15 ml/min. If there are severe uremia symptoms, such as acidosis, electrolyte disturbance, cardiac insufficiency, nausea, vomiting, etc. dialysis may be appropriate in advance.
Peritoneal Dialysis Program
1. Peritoneal dialysate treatment with glucose peritoneal dialysate can cause metabolic disorders such as hyperglycemia; the low pH environment required for the preparation process can cause chronic peritoneal inflammation and damage the peritoneum; after glucose is absorbed, terminal glycation products can be produced in the body (AGEs), AGEs can bind to special receptors on a variety of cells (such as vascular smooth muscle cells, endothelial cells, etc.), resulting in thickening of the blood vessel wall, inducing tissue ischemia and other dysfunctions. Icodextrin dialysate and amino acid dialysate can be used in patients with diabetic nephropathy. The former uses polysaccharide as an osmotic agent, which has the characteristics of long osmotic pressure maintenance, high ultrafiltration efficiency, and less formation of AGEs, and is especially suitable for patients with end-stage diabetic nephropathy. The amino acid dialysate did not contain glucose, and the osmotic pressure was close to that of the 2.5% glucose dialysate (365 mOsm/L vs 396 mOsm/L). It can not only produce ultrafiltration but also directly supplement the nutrients that the human body lacks (each bag of 2L can provide 22g of amino acids), which is suitable for diabetic peritoneal dialysis patients, especially those with malnutrition.
2. Dialysis mode and dialysis dose The choice of peritoneal dialysis regimen and dialysis dose in diabetic patients should be based on peritoneal transport characteristics, and there is no significant difference in peritoneal transport function between diabetic and non-diabetic nephropathy patients with ESRD.
other measures
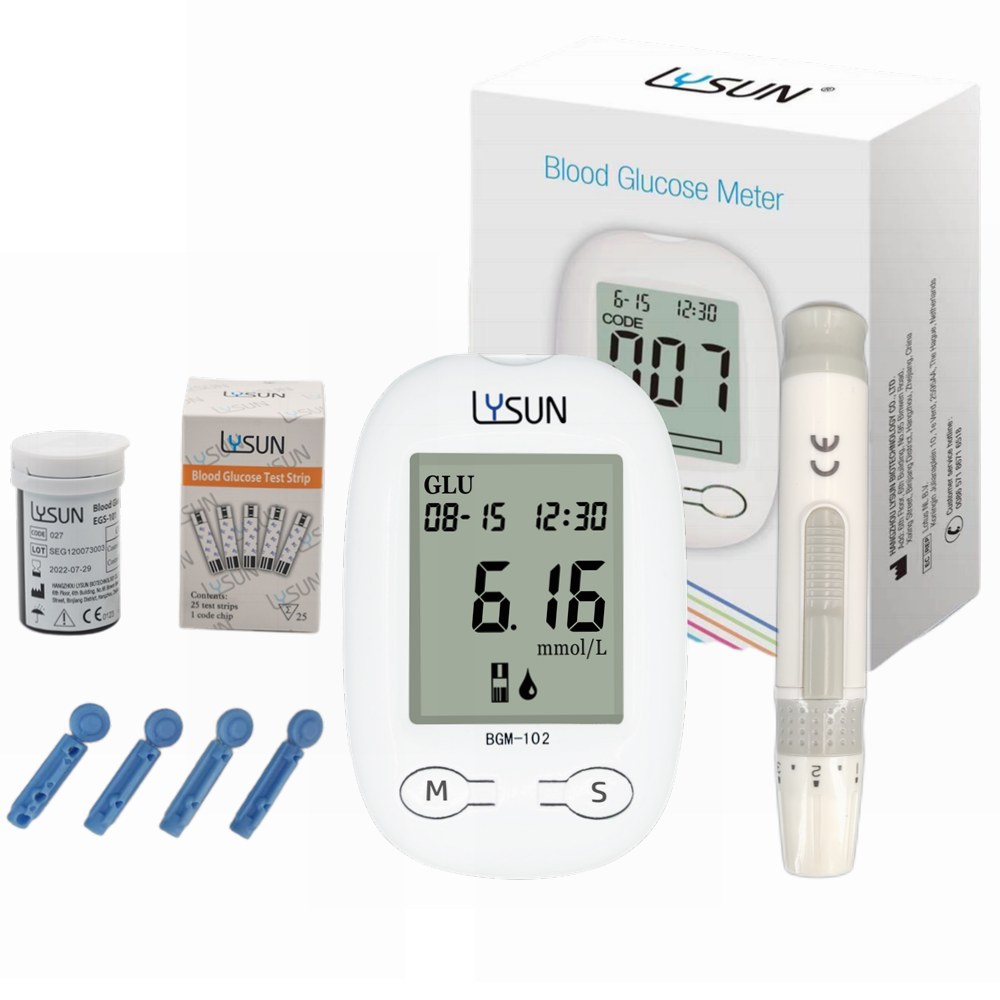
1. Glycemic control: Diabetic peritoneal dialysis patients should, in principle, use insulin to control blood sugar in addition to dietary control.
Diet: To ensure calorie supply, the total daily calories after dialysis are 1800-2000 kcal, with an average of 35kcal/(kg·d), a high-quality protein diet of 1.0-1.2g/(kg·d) is selected, and the intake of water and sodium salt is properly controlled. Supplement with water-soluble vitamins.
Insulin use: Because the dialysate contains a large amount of glucose, dialysis patients need to add an additional 100-200g of glucose load per day, which makes the blood sugar fluctuate greatly during the dialysis treatment. control is more difficult.
Issues to be aware of
1. Target value of blood sugar control: maintain normal blood sugar level during the whole process of fluid exchange, control postprandial blood sugar, and avoid hypoglycemia. Fasting blood glucose should be controlled at around 7.0 mmol/L, postprandial blood glucose should be around 10 mmol/L, and glycosylated hemoglobin <7%.
2. Insulin use: In principle, insulin should be the first choice for all peritoneal dialysis patients, especially CAPD patients. It is recommended to use short-acting insulin, generally not long-acting insulin, because these patients have prolonged insulin half-life (reduced renal clearance of insulin), and long-acting insulin is not conducive to blood sugar control.
3. route of administration: subcutaneous injection and (or) intraperitoneal administration. The former has the advantage of being simple, convenient, and reducing the chance of abdominal infection. However, due to factors such as injection site and concentration, the absorption of insulin is not stable, the blood sugar fluctuates greatly, and hypoglycemia often occurs. The advantage of intraperitoneal administration is that the peritoneum can slowly absorb insulin and enter the systemic circulation through the portal vein, and the process is closer to the physiological mode of insulin release. However, intraperitoneal administration increases the chance of intra-abdominal infection, and the dialysis bag and pipeline will absorb insulin, which affects the efficacy. Patients often need to increase the dosage of insulin (usually 2 to 3 times the dosage of subcutaneous insulin).